Chronic and acute prostatitis – Diagnostic methods
- Preliminary interview
- General physical
- examination
- Rectal examination
- Laboratory tests
- Transrectal prostate ultrasound (TRUS)
- TRUS and acute prostatitis
- TRUS and chronic prostatitis
- Radiological exams
- Cystoscopy
Preliminary interview
(Diagnostic value 10)
We have indicated next to each of the following paragraphs a completely arbitrary score, expressing, according to our experience, the diagnostic capacity of the exam.
It is a fundamental moment in the approach to the prostatic patient, who during the interview, in addition to providing the urologist with specific information on his symptoms, also decides, more or less consciously, whether or not to rely on the doctor in front of him.
The symptoms to investigate are those described in the appropriate section.
I advise doctors who deal with prostatitis pathology to be particularly patient in this diagnostic moment.
The symptoms of prostatitis must be requested several times individually and investigated thoroughly. In our clinic, the symptom questionnaire (see below) is normally submitted to the patient twice in a row, by two different healthcare professionals. Let us remember that most of the time in front of us is a man or boy disheartened or scared both by the chronicity of the disease and by the multiple previous consultations, which have often resulted, from his point of view, in failure or even betrayal. Therefore, sometimes we will tend to underestimate some aspects of the disease in order to overestimate others. It is up to us and our experience to balance the value of the answers.
SYMPTOMS QUESTIONNAIRE
Validated in 2002 at the XVII European Congress of Urology
MINION 0 1 2 3 | ||||
I get up at night | never | 1 time | 2 time | more |
I urinate during the day | over 3 hours | every 2 hours | less than 2 hours | every hour |
Urine comes out | strong | with difficulty | filiform | *** |
| The flow is | regular | irregular | *** | *** |
I drip | absent | present sometimes | always present | *** |
Urgent urination | never | modest | strong | |
PAIN 0 1 2 | ||||
Burning urination | absent | moderate | relevant | *** |
Perineal pain | absent | moderate | relevant | *** |
Inguinal pain | absent | moderate | relevant | *** |
Scrotal tenderness | absent | moderate | relevant | *** |
Coccygeal pain | absent | moderato | relevant | *** |
Suprapubic pain | absent | moderate | relevant | *** |
Anorectal pain | absent | moderate | relevant | *** |
SEX 0 1 2 3 | ||||
Sexual desire | preserved | minus 25% | minus 50% | minus 75%-A |
Erection | preserved | minus 25% | minus 50% | minus 75%-A |
Tempo di ejaculazione | regular | minus 25% | minus 50% | early |
Caratteri ejaculazione | regular | hindered | painful | absent |
Qualità ejaculato | regular | rare | agglutinated | hematic |
Forza ejaculato | regular | decreased | dripping | *** |
General physical examination
Diagnostic value 7
Let's keep in mind that some of the symptoms complained of during prostatitis can instead be caused by other pathologies which must therefore be carefully researched and excluded.
The presence of:
- hernia tip or full-blown inguinal or crural hernias which can cause inguinal or suprapubic tenderness;
- hemorrhoids, perianal fistulas or fissures that can cause anal or perineal tenderness or pain;
- muscle tears, sometimes causing pubalgia or cruralgia in young people;
- epididymitis or varicocele which can cause testicular heaviness and tenderness.
- acquired spinal pathologies (herniated discs, cysts, etc.) or congenital (spina bifida), which can cause the most varied symptoms at the perineal, penile and suprapubic levels
The rectal examination is instead fundamental both to evaluate the level of a possible spasm of the perineal muscles and for the possibility of palpating the emergence of the pudendal nerves whose very severe tenderness is always correlated to an inflammation responsible for generating the Painful Syndrome of the Pelvic Floor.(SEE)
Rectal examination
Diagnostic value 10
I do not think it is useless to underline that the exploring finger must be inserted into the rectum with extreme delicacy, so as not to lose, due to a well-understandable reaction of the patient, the possibility of perceiving a pathological contracture of the muscles of the levator ani. This contraction can also be indirectly hypothesized if there is elective tenderness of the pudendal nerves at the level of the sacrospinal ligament.
It should be noted that the irritation of the pudendal nerves is never primitive but is always secondary both to the chronic reactive contraction of the perineal muscles and to the presence of repeated chronic traumas of the perineum (hard bicycle seat, horse saddle, scooter vibrations etc.). In our case, birth traumas are obviously not part of this negotiation.
For educational reasons, the exploration of the rectum can be divided into inferior (study of the rectal sphincter, the hemorrhoidal area and the muscles of the perineal floor), medium (prostatic apex and body of the prostate) and superior (prostatic base and seminal vesicles).
The maneuver can, after learning, be self-performed by the patient himself, thus being able to independently obtain information on the progress of the disease during treatment. We have also been able to see that this, although naturally not having a strictly therapeutic value, usually involves a decrease in anxiety linked to the disease, making the subject aware of the location of their diseased organ and the starting point of their disorders.
The prostate during prostatitis can appear either enlarged and soft, as in the acute inflammation phase, or volumetrically normal with a regular or hardened consistency. The exam can generate lively pain, which can radiate to the tip of the penis, especially when exploring its inflamed portion. The rectal examination must naturally also be aimed at excluding, especially in less young subjects and with possible haemospermia, the presence of neoplastic formations, absolutely indistinguishable, only with the examination, from calcific nodules or granulomatous prostatitis. In all doubtful cases, therefore, it is necessary to measure the PSA (Prostatic Specific Antigen) in the blood, which can help us, together with the prostatic fusion biopsy (under the guidance of MRI), to resolve the diagnostic doubt.
The exploration must be completed by palpation of the seminal vesicles to appreciate their consistency, their volume and, if present, their tenderness.
Laboratory tests
Diagnostic Value 10
When we began to deal with prostatitis, following the example of other Urologists, we subjected our patients to the four-glass test (Stamey 1968), i.e. looking for inflammatory cells and microbial agents in the urine before and after prostate massage.
This test, although still widely used, has been abandoned by us and replaced by the tests listed below:
- Urine culture and sperm culture with susceptibility testing for common germs, protozoan fungi and saprophytic bacteria, on media enriched for this purpose.
- On urine, semen and urethral swab after prostate massage DNA amplification (with PCR technique), of Chlamydia, Mycoplasma, Gonococci, Herpes virus (HSV) and Papilloma virus (HPV)
- IGG and IGM for Chlamydia and Mycoplasma and secretory antiChlamydia IGa.
If we suspect that the partner is also infected, we ask:
- Vaginal swab with research, culture and possible antibiogram for common bacteria, fungi and protozoa, and amplification of the DNA of Chlamydia, Mycoplasma, Gonococci, Herpes virus and Papilloma virus. Note that some strains of HPV in women can be potentially highly carcinogenic!
In the presence of sexual symptoms we require a series of hormonal dosages such as:
- Total testosteroneemia
- Free testosterone
- DEHA and DEHAS
- LH, FSH, Prolactin
- 17 Beta estradiol
- Total PSA
In the presence of suspected subfertility we request:
- Spermiogram
- Nemasperm penetration test
- Post Coital Test (PCT)
Transrectal prostate ultrasound
Diagnostic value 10
The ultrasound study of the prostatitis patient is a fundamental moment in the diagnostic and, as we will see, therapeutic process of the disease. But this study must be carried out in the right way and with the appropriate equipment. The patient must be studied with a full bladder (but not overfilled!) and transrectally, with a basal phase and a so-called phase. dynamic, i.e. during urination. In our experience we prefer to carry out the investigation with the patient standing, in order to then facilitate the execution of urination under ultrasound vision by combining it with uroflowmetry. For this purpose, the ultrasound probe must be of the thin new generation type so as not to create abnormal compressions on the bladder neck. There must be at least two prostate exploration planes (biplane or multiplane probe) and the vibration frequency of the crystals must be between 7 and 10 MHz.
Only with these prerogatives can we be sure of studying the organ adequately.
The ultrasound patterns to be taken into consideration in the basal phase are the following:
- Gland volume
- Capsular profile
- Echogenicity of the glandular tissue
- Absence or presence of fibro-calcific formations
- Regularity of the course and echogenicity of the ejaculatory ducts
- Caliber of the veins of the periprostatic plexus
The ultrasound patterns to be taken into consideration in the dynamic voiding phase are the following:
- Profiles and reflectance of the bladder floor (trigon)
- Elasticity and morphology of the bladder neck
- Distensibility of the prostatic urethra
- Profiles and reflectance of the walls of the prostatic urethra
- Profile and reflectance of Veru montanum
- Any urethro-prostatic reflux can be highlighted with the aid of color Doppler
Transrectal prostate ultrasound (TRUS) and acute prostatitis
In acute inflammation, the gland may have a regular or increased volume and with preserved or less symmetry of the two lobes.
- Ultrasound in the mild forms initially shows a hypoechoic periurethral halo resulting from glandular edema.
- As the disease progresses, intraglandular hypoechoic streaks appear resulting from the dilation of the blood vessels which is sometimes associated with the dilation of the periprostatic venous plexus of Santorini.
- In the more severe forms the gland increases in volume while increasingly large portions of tissue become hypoechoic due to wider inflammatory tissue involvement. This situation, in older subjects or those with decreased immunoresistance, can evolve into a prostate abscess whose ultrasound picture in the initial phase is typically represented by a transonic area with irregular margins
Transrectal prostate ultrasound (TRUS) and Chronic prostatitis
Chronic prostatitis is an inflammatory process affecting the prostate, a very common pathology that can be caused by various factors. It is estimated that annually, approximately one third of the male population is affected by prostatitis. Different types can be distinguished, acute, bacterial, asymptomatic inflammatory, but chronic abacterial prostatic is certainly the most widespread.
Chronic prostatitis presents fluctuating symptoms, with acute periods and phases of improvement, requiring different treatments based on the level of severity. The therapies for the treatment of chronic prostatitis are assigned following an accurate diagnosis, consisting of digital rectal examination, culture of prostatic secretion, spermiogram, transrectal ultrasound (TRUS) and PSA measurement. While the first three tests are indicated for a first diagnostic approach and to provide information on prostatic functionality, TRUS and PSA, by carrying out detailed anatomical-structural analyses, are also considered means of preventing prostate cancer.
Now let's see what ultrasound changes the different portions of the prostate undergo during chronic prostatitis:
PROSTATIC CAPSULE AND GLANDULAR PARENCHYMA
The prostatic capsule and glandular volume are usually regular.
Ultrasound alterations of the glandular parenchyma can be localized in the periurethral or peripheral area or ubiquitous. In chronic inflammation of modest entity, it is essential, as specified above, to use a high resolution ultrasound probe, in order to better detect the milder signs of the disease, initially consisting of areas with irregularly oval hyper- or hypoechoic margins. There is sometimes a reactive dilation of the periprostatic veins, which is not specifically diagnostic. In the most serious chronic inflammations we can detect three types of echogenic response of the glandular parenchyma:
1. areas with hypoechoic structure with blurred boundaries in the surrounding parenchyma (Hypoechoic Prostatitis – photo 4).
2. areas with a homogeneously hyperechoic structure with typically serrated and well-defined margins (Hyperechoic Prostatitis – photo 5).
3. areas with a significantly hyperechoic structure, sometimes with the presence of a hypoechoic halo of surrounding acute glandular reaction.
FIBROCALCIFICATIONS
They are highly hyper-reflective areas with both a rounded and irregularly oval shape with diameters from a few millimeters (so-called "lime spray"), up to a few centimetres; they can be subtended, depending on their density, by a rear shadow cone.
A distinction must be made on the diagnostic value of this finding, depending on the age of the patient. While calcifications located at the periphery of a prostatic adenoma, in the elderly patient, are attributable to precipitations of minerals within acini or ducts compressed by the adenoma itself, and therefore usually do not generate any symptoms, in the young this type of the lesion can be associated either with ongoing prostatitis or with outcomes thereof which are therefore devoid of pathological significance.
Typically in young patients, calcification is localized for anatomical reasons, usually in the periurethral area, due to the precipitation of crystals inside periurethral acini whose ducts have become obliterated due to an inflammatory situation.
In reality, calcifications are almost never true calcifications (to be understood as a kidney stone), but are very tenacious but labile aggregates, which in the case of important recurrent infections must be infiltrated and sterilized to obtain a good therapeutic result (see film ).
On the one hand, calcifications can be an important cause of some prostatitis symptoms (premature ejaculation, haemospermia) and on the other they can maintain, if present, the infection, "defending" microbial agents within them, as in a fortified citadel. cause of reinfections by forming the so-called bacterial biofilms. Recent research (Daniel Shoskes of Cleveland University) has documented the presence of nanobacteria within these calcifications. Hence the implementation of some therapeutic protocols based on EDTA+tetracycline suppositories.
The symptoms associated with the presence of calcifications are different depending on their location:
1. periurethral subcervical: urination disorders; stabbing pain on the tip of the penis at the beginning and/or at the end of urination.
2. Median perineal: perineal tension or no discomfort.
3. perimontanal: premature ejaculation; pain on ejaculation; sensation of obstacle to the escape of sperm; haemospermia (Prostatic Calcification – photo 6).
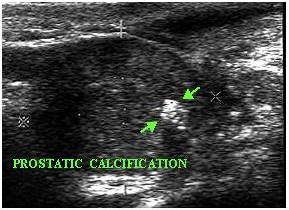
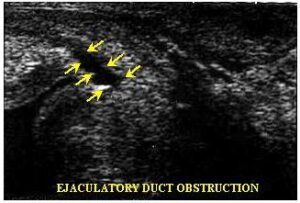
4. peri or intraductal (ejaculatory ducts): symptoms same as those of perimontane localization (Ejaculatory Duct Obstruction – photo 7).
As already mentioned, these calcifications usually contain a high quantity of urates, creatinine, xanthines and uridine and on this basis some authors have experimentally tried to cure prostatitis by administering antiuric substances generally, concluding at the end of the research that a fair improvement in symptoms was achieved, but as long as the drug was administered!
EJACULATORY DUCTS
In the normal state, they can be highlighted on ultrasound, especially in the dynamic voiding phase, as two hypoechoic striae (visualised individually with the probe in linear scanning), which converge towards the Veru Montanum. In the presence of acute inflammation they are more evident due to the parietal edema which accentuates their visibility. In conditions of chronic inflammation the walls often become hyperreflective due to their thickening and fibrosis. Sometimes parietal fibrosis is associated with intraluminal stones that can be seen as sonolucent spots positioned circularly "like rosary beads".
Symptoms associated with inflammation of the ejaculatory ducts manifest themselves during orgasm with pain or burning upon ejaculation, sometimes hemospermia, sensation of obstruction with decreased quantity and altered quality of ejaculated sperm, up to the absence of ejaculation.
SEMINAL VESICULES
In the normal state they are clearly visible (especially after sexual abstinence) in continuation with the prostatic base, as two hypoechoic ovary formations, with hyperechoic septa inside. A situation of inflammation usually causes their dilation due to their failure to empty following the obstruction by inflammatory edema of the ampulla or ejaculatory ducts. Ultrasound findings are similar to the presence of cysts and can be mono or bilateral. Sometimes during significant chronic inflammation (e.g. from trichomonas or gonorrhea), the vesicles appear sclerotic and with hyperreflective walls. The inflammation of the vesicles usually manifests itself laterally on the two sides of the pubis, with a dull and continuous pain which can intensify during defecation, so as to produce a reflex constipation, which, with a vicious circle will further increase the consistency of the stool and therefore the pain as they pass.
Due to their shape, they are often the last anatomical structure to heal during inflammation and therefore their treatment must be carried out with particular care.
URICLE
It is normally an involuted anatomical formation and therefore not ultrasound-visible. Sometimes, however, it remains present and can dilate and form a cyst, which can be highlighted ultrasoundally as a median paraurethral asonic area. This situation can sometimes remain completely asymptomatic, while other times it can generate a painful situation that can be resolved with appropriate therapy.
BLADDER NECK AND TRIGONE
The functional ultrasound study of this region is only possible in the dynamic voiding time.
In normal subjects, the beginning of urination is characterized by the funneling of the neck in its anterior and posterior component, in a soft and homogeneous manner, to draw a truncated cone with its base pointing towards the bladder and the apical portion continuing in the urethra (photo 9).
In the presence of sclerosis (or dysectasia), ultrasound shows a slow opening of the neck which no longer appears soft, but stiffened (snap opening), with the appearance of a noticeable endoluminal protrusion of the posterior portion (posterior lip). The physiological funneling is thus altered (Bladder Neck Sclerosis – photo 8) and the space for urine to flow into the urethra is significantly reduced with consequent acceleration of the urine itself (possible urethro-prostatic reflux).
In this pathological situation, the closure of the neck is also altered, as it does not occur gradually, but, as for the opening, "in a snap", leaving a small quantity of urine trapped in the urethra which will flow outside, after the end of urination, causing a typical drip. The existence of this anatomical situation is, as explained in the physiopathology, a cause to be removed to prevent the perpetuation of chronic prostatitis.
Inflammatory alterations of the trigone (trigonitis), whether primary or secondary, are poorly identifiable with ultrasound unless they are very evident and characterized by the presence of mucous extrusions (papillary trigonitis), visible as many very small digitations in the bladder wall.
URETHRA
Like the bladder neck, the urethra is also visible ultrasound only in the dynamic voiding phase and only in its first portion (prostatic and membranous urethra).
In the normal subject, the funneling of the neck is followed by the soft distension of the prostatic urethra whose caliber does not usually exceed 10 mm. The walls appear thin and slightly more reflective than the surrounding glandular tissue (photo 9).
In urethritis the distension appears rigid and the walls noticeably hyperreflective, thickened and with an irregular profile. In the case of narrowing (stenosis) of the urethra downstream of the portion that can be explored with transrectal ultrasound, the appreciable indirect symptom is hyperdilation in its prostatic portion, without other signs of disease (photo 10). In these cases, a radiological study of urination with retrograde urinary urethrocystography will be necessary.
Radiological exams
Diagnostic value 10 (only if actually necessary!)
In patients suffering from chronic prostatitis, if urethral stricture has been suspected, the only useful radiological examination is voiding retrograde urethrocystography. This test allows, during the instillation of radiopaque contrast liquid into the urethra, to study both the course and caliber of the urethra itself and the bladder. In the subsequent voiding phase, it allows us to study the dynamics of the opening of the bladder neck in order to highlight or exclude any sclerosis of the same.
It is therefore an irreplaceable investigation to perform for a suspected urethral stricture.
Cystoscopy
(diagnostic value 0-1)
In our experience, the cystoscopic study of the prostatic patient is completely useless as it does not add other information to that obtainable with the other diagnostic methods already described. Indeed, many patients report a sharp worsening of symptoms after undergoing this test!
The execution of this examination, however, but only as an initial stage of an endoscopic intervention (e.g. resection of the neck or unblocking of a urethral stricture), highlights in the case of urethro-prostatitis, the urethral duct and the bladder neck are very red and with dilated and easily bleeding blood vessels.
At the level of the prostatic lodge, blackish clods can often be seen transparently, attributable to stones within the periprostatic acini. Still in the lodge, in the presence of urethro-prostatic reflux, the wall of the urethra loses its pink color to become mother-of-pearl-greyish due to chronic inflammatory phenomena, which have evolved into fibrosis. Naturally, due to the loss of its physiological elasticity, this portion of the urethra will cause burning sensations when passing urine.

